WHAT: Reflexive and Indirect Techniques in Manual Medicine
For Pain Relief, Spinal Alignment, and Joint Freedom
Workshop II
WHEN: August 29, 2010
TIME: 10 am to 3 pm
WHERE: The Holiday Inn Galleria Suites, Ortigas Center, Pasig, Philippines
EXPECT: To walk away with basic and intermediate tools for a working Integration of Muscle Energy, Reflexive Releases, and Articulatory Techniques that you can use the very next day at your clinics.
The study group will go over The Location and Uses of Reflexive Points.
REFUND POLICY: Try out the techniques and principles for 60 days. If, within that time, your clinical application of the technology has not (a) allowed you to turn off pain and (b) recovered your investment in the course, we will refund your money.
CE: The workshop counts as 6 coursework hours toward certification as an RDT practitioner. Certificates will be furnished. Participants may choose to test for certification as RDT Associate Practitioners or RDT Practitioners – Level I.
PREP: Please come in loose and repositionable clothing.
COST SHARING:
Late Reg: P2,000 if prepaid by Friday, August 06, 2010
On-Site Registration: P2,500
P500 waived from cost-shares for the following:
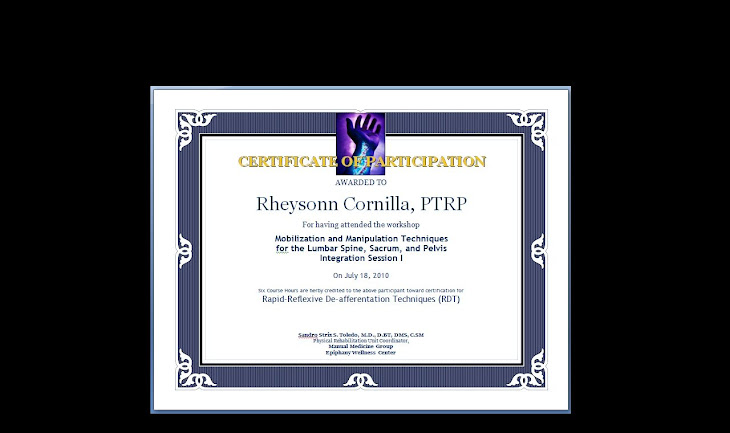
MMG Workshop participants (any workshop from 2007, just bring your certificate);
SOMATIC members, Bowen Practitioners, and FITPRO members.
Credit card processing via Paypal is accepted.
Delayed or deferred sharing may be arranged. We just want to know who’s coming.
Early Course Outline may be requested via email.
Contact Rheysonn at +63 922 7914724 to confirm participation or request more info.
Please furnish email addresses and return contact numbers.
What is the technology behind R.D.T.s?
Reflexive Antagonism is the phenomenon by which muscles with opposing functions tend to antagonistically inhibit each other. When one muscle is activated, its opposite muscle or muscle group or is reflexively inhibited or deactivated. By example, when the triceps brachii is stimulated, the biceps muscle on the same extremity is reflexively inhibited.
The phenomenon of Relfexive Antagonism is now known to be fleeting, incomplete, and weak. The incompleteness of the effect is related to postural and functional tone. Also, reflexes in vivo are polysynaptic, with entire muscle groups responding to noxious stimuli (Nociceptive Reflex or Nociceptive Withdrawal Reflex).
Reflexive antagonism is the basic original notion behind indirect muscle energy techniques. While this notion is now understood to be incomplete, the clinical mechanism of Reflexive Antagonism continues to be useful in widespread Osteopathic and OMT-derived practice. Reciprocal Inhibition is a synonym. (See Entry under Muscle Energy Techniques)
Techniques that utilize reflexive antagonism, (such as Rapid De-Afferentation Techniques) are manual medicine techniques and protocols that utilize reflexive pathways and the phenomenon of reciprocal inhibition as a means of switching off inflammation, pain, and protective spasm for entire synergistic muscle groups or singular muscles and soft tissue structures.
From http://www.amazines.com/Reflexive_Antagonism_related.html and http://en.wikipedia.org/wiki/Reflexive_antagonism
Suggested reading:
1. Fryer G 2000 Muscle Energy Concepts –A Need for a Change. Journal of Osteopathic Medicine. 3(2): 54 – 59
2. Fryer G 2006 MET: Efficacy & Research IN: Chaitow L (Ed) Muscle Energy Techniques (3rd edition) Elsevier, Edinburgh
3. Ruddy T 1961 Osteopathic rhythmic resistive duction therapy. Yearbook of Academy of Applied Osteopathy 1961, Indianapolis, p 58
4. Solomonow M 2009 Ligaments: A source of musculoskeletal disorders. J Bodywork & Movement Therapies 13(2): IN PRESS
5. Smith, M., Fryer, G. 2008 A comparison of two muscle energy techniques for increasing flexibility of the hamstring muscle group Journal of Bodywork and Movement Therapies 12 (4), pp. 312-317
6. McPartland, J.M. 2004 Travel trigger points - Molecular and osteopathic perspectives Journal of the American Osteopathic Association 104 (6), pp. 244-249
7. Hamilton, L., Boswell, C., Fryer, G. 2007 The effects of high-velocity, low-amplitude manipulation and muscle energy technique on sub occipital tenderness International Journal of Osteopathic Medicine 10 (2-3), pp. 42-49
8. McFarland, J.M. 2008 The endocannabinoid system: An osteopathic perspective Journal of the American Osteopathic Association 108 (10), pp. 586-600
9. Magnusson M Simonsen E Aagaard P et al. 1996a Mechanical and physiological responses to stretching with and without pre-isometric contraction in human skeletal muscle Archives of Physical Medicine & Rehabilitation 77:373-377
10. Magnusson M Simonsen E Aagaard P et al. 1996b A mechanism for altered flexibility in human skeletal muscle. Journal of Physiology 497(Part 1):293-298