Thursday, February 14, 2013
Friday, December 16, 2011
Dry Needling for Somatic Pain (Trigger Points): on the "Efficacy of specific needling techniques in the treatment of myofascial pain syndrome"
SITE NOTES:
still reviewing meta data.
this study is in review.
posted temporarily for discussion purposes.
Efficacy of specific needling techniques in the treatment of myofascial pain syndrome
Candice Brunham
Kelly McNabney
Jody Wiebe
Jeff Norwood
Research Supervisors:
Dr. Darlene Reid
Dr. Babak Shadgan
Needling Intervention + Adjunct Therapy vs Adjunct Therapy vs Control
• Comparison of superficial DN + stretching vs stretching vs control (Edwards & Knowles, 2003):
– No significant difference between
groups immediately post
treatment
– Superficial DN + stretch favoured
at follow up for increase in PPT
Discussion – Needling vs Needling Intervention
• No trends seen due to heterogeneity
of studies
– Study by Irnich et al (2002)
found acupuncture
to be significantly more effective than DN
– Ceccherelli et al (2002)
found deep
acupuncture to be more effective than
superficial acupuncture
– Birch & Jamison (1998)
found relevant acupuncture to be more effective than irrelevant acupuncture
• Future studies comparing needling
techniques are needed to determine
the most effective technique
Discussion – Needling vs
Other Intervention
• Studies which favoured lidocaine injection
over DN techniques involved only one
treatment session
• Study by Ga et al (2007)
which favoured
IMS over lidocaine injection had 3
treatments over 3 weeks
• The form of dry needling may play a role in
treatment efficacy
• Study by Ilbuldu et al (2004)
favoured
laser over DN, but subjects received a
greater number of laser treatments
Implications for Practice
• Best practice involves a structured
interdisciplinary approach including
physical and cognitive behavioral strategies
• The national institute of health (USA)
consensus statement on acupuncture
(1997) concluded that it may be useful as
an adjunct treatment
• This review indicates a need for future
investigation of dry needling therapies as
part of a comprehensive program
Conclusions
• No clear evidence that Dry Needling techniques are more efficacious than placebo, sham, or alternative treatment techniques
• No clear recommendations can be made regarding
the most effective needling technique or optimal
length and frequency of treatment
• Results suggest that multiple treatment sessions are
more effective on pain outcomes than single
treatment sessions
• Level of evidence does not exceed moderate
Acknowledgements:
Dr. Darlene Reid, Dr. Babak Shadgan,
Charlotte Beck, Dr. Angela Busch, &
Meredith Wilso
still reviewing meta data.
this study is in review.
posted temporarily for discussion purposes.
Efficacy of specific needling techniques in the treatment of myofascial pain syndrome
Candice Brunham
Kelly McNabney
Jody Wiebe
Jeff Norwood
Research Supervisors:
Dr. Darlene Reid
Dr. Babak Shadgan
Needling Intervention + Adjunct Therapy vs Adjunct Therapy vs Control
• Comparison of superficial DN + stretching vs stretching vs control (Edwards & Knowles, 2003):
– No significant difference between
groups immediately post
treatment
– Superficial DN + stretch favoured
at follow up for increase in PPT
Discussion – Needling vs Needling Intervention
• No trends seen due to heterogeneity
of studies
– Study by Irnich et al (2002)
found acupuncture
to be significantly more effective than DN
– Ceccherelli et al (2002)
found deep
acupuncture to be more effective than
superficial acupuncture
– Birch & Jamison (1998)
found relevant acupuncture to be more effective than irrelevant acupuncture
• Future studies comparing needling
techniques are needed to determine
the most effective technique
Discussion – Needling vs
Other Intervention
• Studies which favoured lidocaine injection
over DN techniques involved only one
treatment session
• Study by Ga et al (2007)
which favoured
IMS over lidocaine injection had 3
treatments over 3 weeks
• The form of dry needling may play a role in
treatment efficacy
• Study by Ilbuldu et al (2004)
favoured
laser over DN, but subjects received a
greater number of laser treatments
Implications for Practice
• Best practice involves a structured
interdisciplinary approach including
physical and cognitive behavioral strategies
• The national institute of health (USA)
consensus statement on acupuncture
(1997) concluded that it may be useful as
an adjunct treatment
• This review indicates a need for future
investigation of dry needling therapies as
part of a comprehensive program
Conclusions
• No clear evidence that Dry Needling techniques are more efficacious than placebo, sham, or alternative treatment techniques
• No clear recommendations can be made regarding
the most effective needling technique or optimal
length and frequency of treatment
• Results suggest that multiple treatment sessions are
more effective on pain outcomes than single
treatment sessions
• Level of evidence does not exceed moderate
Acknowledgements:
Dr. Darlene Reid, Dr. Babak Shadgan,
Charlotte Beck, Dr. Angela Busch, &
Meredith Wilso
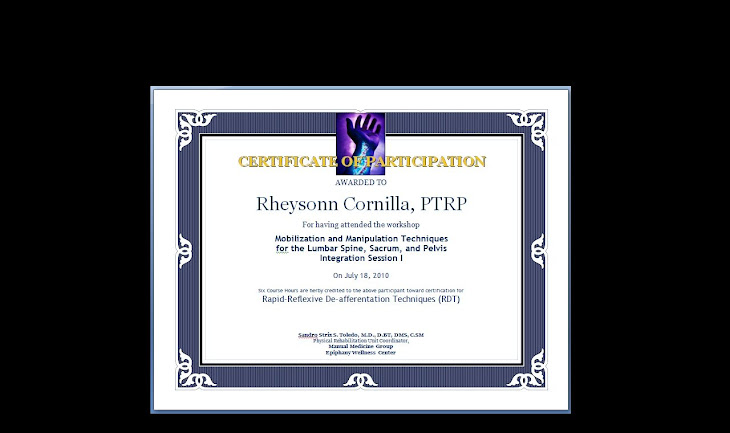
Sunday, December 4, 2011
RSD
[Case:
Complex Regional Pain Syndrome
( Reflex Sympathetic Dystrophy )
This is a constellation of symptoms springing from increased sympathetic tone at one or more extremities. Pain, erythema, and edema are seen. Lymphedema and fascial strains may be noted along the extremities. This may occur after blunt force Trauma, a crush or fall injury, or surgery.
We see a sympathetic overload. Changes in tissue circulation occur. Tender points, tissue changes, or vertebral rotations are noted over T5-7, T10-L2. Motor and tissue changes may be seen along C4-T1 or L1-S3. Compensatory patterns over unaffected areas may be noted.
The complex is fairly responsive to Reflexive De-Afferentation Techniques, OMT, and manual drainage techniques.
www.manual.blogspot.com]
Complex Regional Pain Syndrome
( Reflex Sympathetic Dystrophy )
This is a constellation of symptoms springing from increased sympathetic tone at one or more extremities. Pain, erythema, and edema are seen. Lymphedema and fascial strains may be noted along the extremities. This may occur after blunt force Trauma, a crush or fall injury, or surgery.
We see a sympathetic overload. Changes in tissue circulation occur. Tender points, tissue changes, or vertebral rotations are noted over T5-7, T10-L2. Motor and tissue changes may be seen along C4-T1 or L1-S3. Compensatory patterns over unaffected areas may be noted.
The complex is fairly responsive to Reflexive De-Afferentation Techniques, OMT, and manual drainage techniques.
www.manual.blogspot.com]
Subscribe to:
Comments (Atom)